Diagnostic tests
Vital stains (fluorescein, rose bengal, lissamine green)
Schirmer test
OSA VET Ocular Surface Analyzer
Biography
Impression cytology
Treatment
Depending on the cause and the characteristics of the patient, dry eye may require different custom-designed treatments. Beyond artificial tears (preferably made with hyaluronic acid and without preservatives) and lubricating ointments, there are in-office treatments that effectively contribute to improving symptoms:
Eyelid hygiene: Apply heat to the eyelids, massage them and clean them with soap solution, gels, or specific wipes. This removes excess bacteria and secretions.
Environmental measures: Avoid heating, air conditioning, fans, and polluted or dusty environments. Use humidifiers.
Protect the eyes with goggles.
Moisturize the eyes with artificial tears.
Consume fatty acid supplements, especially omega 3, in high doses to improve tear quality.
Administer anti-inflammatories or topical antibiotics or orally, under the prescription of the specialist.
Specific stem cell treatments.
Surgeries such as buccal mucosa graft or Stenson’s duct transposition.
The vicious circle of dry eye.
As it is a chronic disease, the dry eye treatment does not end when you leave the office but requires a series of care and habits that must be carried out at home.
In which animals is it more frequent?
Dry eye is more common in older patients.
There are more predisposed breeds, such as flat-nosed or brachycephalic dogs (French Bulldog, English Bulldog, or Carlino), which can suffer from the dry eye when they are only a few years or months old.
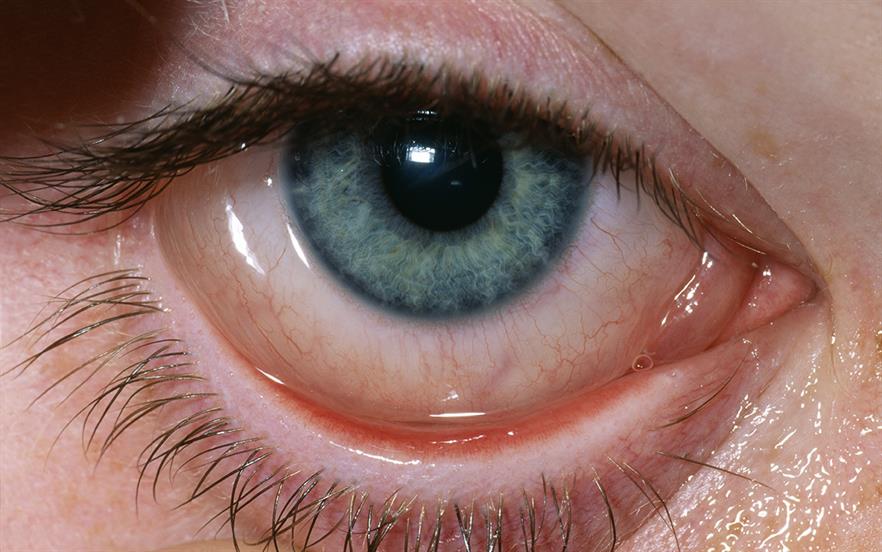
Dry eye syndrome is a common condition caused by a chronic deficit of lubrication and moisture on the eye’s surface due to insufficient tear production.
With each blink, the tears are distributed through the most superficial layer of the eye (cornea), providing lubrication, reducing the risk of infection in the eyes, and eliminating foreign bodies.
Request Information without Compromise
I have read and accepted the information on data protection provided on the Web, and I authorize them to contact me to offer me products and services related to those requested and to retain me as a customer.
What is the cause of dry eye?
An adequate and even layer of tear on the eye’s surface is essential to maintain good vision.
A normal tear film consists of three components:
An oil component (lipid)
An aqueous component (aqueous)
A component similar to the mucosa (mucin)
Dry Eye
Different glands produce each component of tear in or near the eye:
The meibomian glands produce the oil component in the eyelids.
The lacrimal glands produce a watery component.
The mucin component is produced by goblet cells in the conjunctiva.
A problem with any of these sources of tear film components can lead to dry eyes.
Age: Dry eyes are part of the natural aging process. Most people over the age of 65 can have symptoms.
Gender: Women are more likely to develop dry eyes due to hormonal changes caused by pregnancy, use of oral contraceptives, and menopause.
Medications: Antihistamines, nasal decongestants, antihypertensives, and antidepressants can reduce tear production.
Medical conditions: People with rheumatoid arthritis, diabetes, and thyroid problems are more likely to have symptoms of dry eyes.
Environmental conditions: Exposure to smoke, wind, and dry climates can increase the evaporation of tears and cause dry eye symptoms. Not blinking regularly, such as working with computer screens for long periods, can also contribute.
Dry eye symptoms
“Pinch” or foreign body sensations, eye fatigue or pain, itching, difficulty blinking, eye redness, photophobia (sensitivity to light), and blurred vision.
The consequences of dry eye syndrome range from subtle but constant eye irritation to significant inflammation and even scarring on the eye’s surface.
Dry eye treatment
The specific type of dry eye will determine the type of treatment your ophthalmologist recommends to relieve your symptoms.
Among the different treatment options are:
Artificial tears.
Tear plugs: The tear ducts can be blocked with small silicone or gel plugs that can be removed, if necessary.
Dry Eye
Acid nutritional supplement
Omega-3 Fatty: Helps increase tear production.
Treatment of inflammation of the ocular surface or eyelid.
Self-care: Regularly blinking when reading or looking at a computer screen for long periods, increasing humidity in the air at work and home with humidifiers, wearing sunglasses, and nutritional supplements that contain essential fatty acids.
In cases of complete involvement of the limbus in which there are no stem cells to repopulate the corneal surface, a conjunctival limbal autograft can be considered, obtaining the donor limbus from the other eye (in case of involvement of only one eye).
Treatment of cases involving both eyes involves a donor-obtained keratolimbar allograft procedure.
Cultured stem cells have also been used to create grafts and transplant them into patients with limbic insufficiency.
What is dry eye syndrome?
Dry eye is a syndrome that causes discomfort and discomfort in the eyes, visual problems, and, in some cases, lesions on the ocular surface, affecting the cornea and the conjunctiva. It can have different degrees of severity due to instability or alteration of the tear film, either due to poor tear production or excessive evaporation. In addition, the diagnosis is usually associated with different degrees of inflammation.
It is a multifactorial, complex, and chronic condition, which is important to address in a personalized way in each patient to offer the best solution, attending to the causes that have triggered it.
From the clinician’s point of view, Dry Eye diseases, included in the tear film dysfunction syndrome, have multiple etiological causes, different combinations of pathological affectations, and different degrees of severity. The embryologist must know these three parameters, quantify them, and establish the appropriate treatment for them. To this end, the present clinical classification has been elaborated, which firstly includes an etiological classification in age, hormonal, pharmacological, immunometric, hyponutritional, dysgenetic, inflammatory, traumatic, neurodeprivative, and tantalic causes, each of these groups including numerous variants. Second is a histopathological classification or ALMEN, an acronym for acuodeficiency, lipodeficiency, immunodeficiency, epitheliopathy, and other non-ocular exocrine glands. And thirdly, a classification of severity in five steps: subclinical (symptoms in situations of overexposure), mild (symptoms usually), moderate (reversible symptoms and signs), severe (irreversible symptoms and signs), and disabling (irreversible loss of vision for corneal damage)